About Us
In an era where assistance often doesn't measure up, TripSit emerges as the beacon of hope. We're driving forward with a mission to dismantle misconceptions about drug use and arm individuals with the tools they need for safer experiences.
Our foundational principles are clear-cut:
- Accept that people will use substances, regardless of legality or social stigma.
- Know it is possible to use substances while reducing harmful practices.
- Conviction that informed education is the cornerstone for harm mitigation.
At TripSit, our emphasis lies in fostering open conversations and enacting harm reduction methodologies. Beyond championing essentials like test kits, we provide a roadmap for more prudent drug interactions. We've cultivated a platform that promotes discourse from scientific, medical, and philosophical angles on drugs, offering counsel rooted in our shared journeys.
Years of Service
Discord Members
Drugs in our Database
Subreddit Subscribers
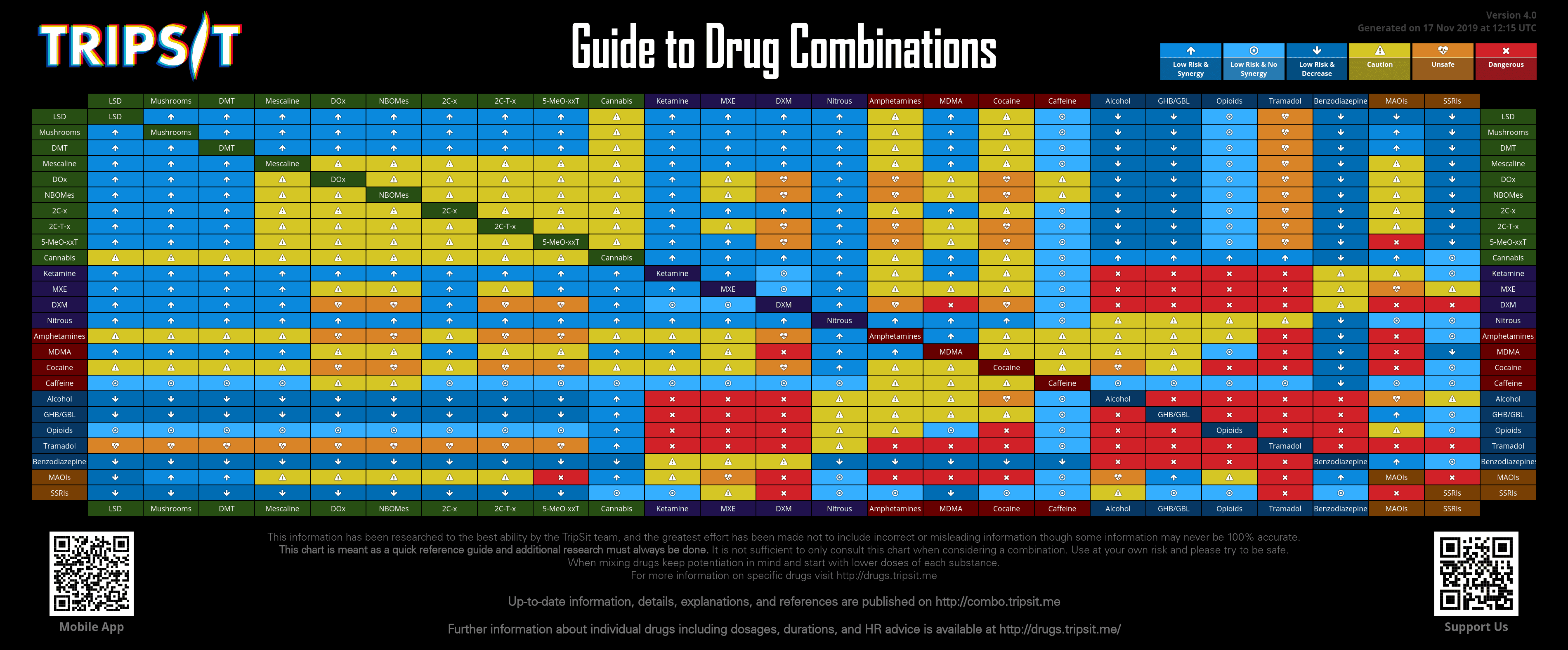
Our Combo Chart is a cornerstone of the HR scene.
We give permissions to print and distribute our chart for non-profit usage.
Full details of usage rights are in our FAQ below, but it boils down to:
- Do not make a profit off our work. We don't do this for profit and neither should you.
- Keep our logo on the chart. We don't ask for money, but we deserve the recognition.
- Do not change the data. We worked hard on this and can't verify adjustments.
Otherwise, we give permission to print out and distribute this chart to whoever wants to. Make your own posters, print it on a t-shirt, or even make a giant banner and display it as a festival! We just want the information out there where it can help people.
Testimonials
We are so proud of our volunteer force and the work they do! The amount of empathy, compassion and knowledge they bring to the table is astounding. We are so lucky to have them!
Resources
TripSit offers various resources, all free of charge, and maintained by the community.
Drug Factsheets
Dive into our comprehensive Drug Factsheets for concise and essential insights on various substances.
Join Our Mission
At TripSit, we're a close-knit, volunteer-driven community. Whether you bring technical prowess, a knack for research, or simply a friendly spirit to chat in the lounge, there's a place for you here. Our ongoing development projects always welcome an extra pair of hands, and our drug databases eagerly await updates with the latest substances. Every piece of information benefits from meticulous review and proofreading. No contribution is too small, and every effort is deeply valued!
Frequently Asked Questions
Answers to our most commonly asked questions. Is your question not here? Contact us using a method below!